Article by Lalita Panicker, Consulting Editor, Views and Editor, Insight, Hindustan Times, New Delhi
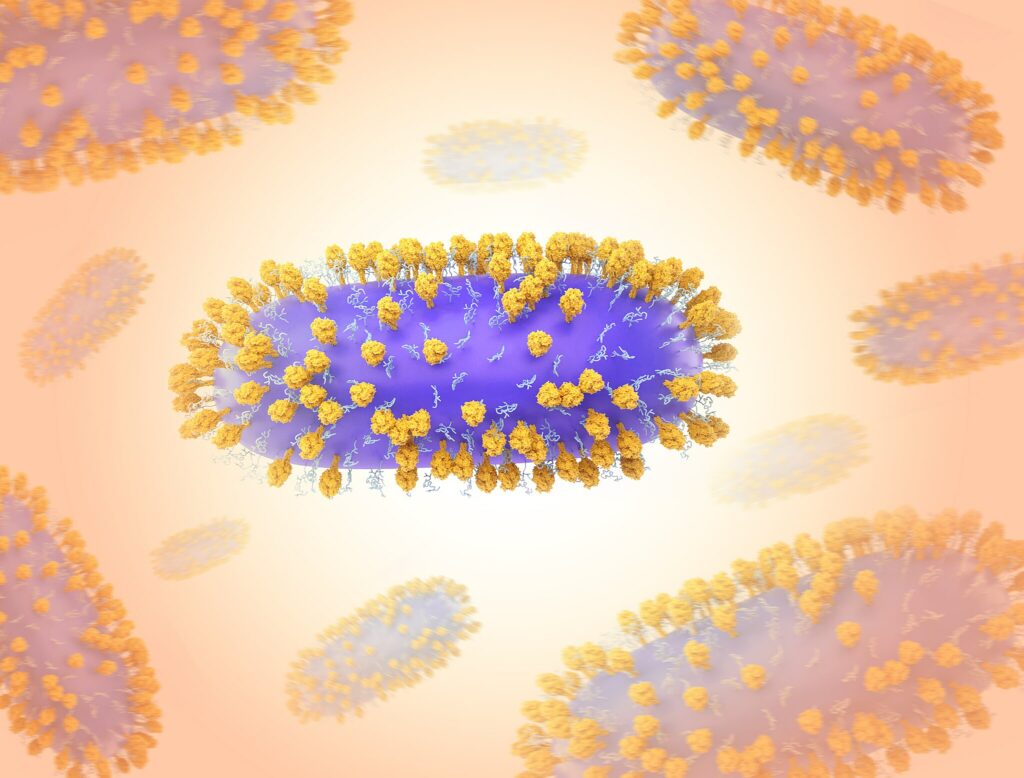
The U.S. Food and Drug Administration (FDA) has approved a vaccine given to pregnant women to protect babies from respiratory syncytial virus (RSV). The virus causes severe lung infections that are the leading cause of U.S. infant hospitalizations. https://www.science.org/content/article/rsv-vaccine-scientific-advisory-panels-and-biodiversity-hot-spot-risk?
Pregnant people who receive the vaccine, called Abrysvo and made by Pfizer, can pass protective antibodies to their foetuses before birth. In July, the FDA approved another tool against RSV, the monoclonal antibody nirsevimab (Beyfortus), a product made through a joint effort by Sanofi and AstraZeneca, which is given during the first year of life.
///
Researchers have accomplished what was once considered an impossible task: fully sequencing not just one Y chromosome, but dozens of them from men from around the world. https://www.science.org/content/article/rsv-vaccine-scientific-advisory-panels-and-biodiversity-hot-spot-risk?
When a first draft of the human genome was unveiled 20 years ago, this stubby piece of DNA that makes males male proved much harder than the rest to sequence because it had so many repetitive and inverted regions. Last week in Nature, researchers report cracking the code using newer technologies. Separately in Nature, a second team reports sequencing 43 more Y chromosomes collected from 21 populations. The team describes high variation in some features, such as the size of the repetitive regions. Whether this affects men in any way has yet to be determined, but one thing is clear: “The Y really is as weird, and as interesting, as we thought,” says Jenny Graves, an evolutionary geneticist at La Trobe University who was not involved in the studies.
///
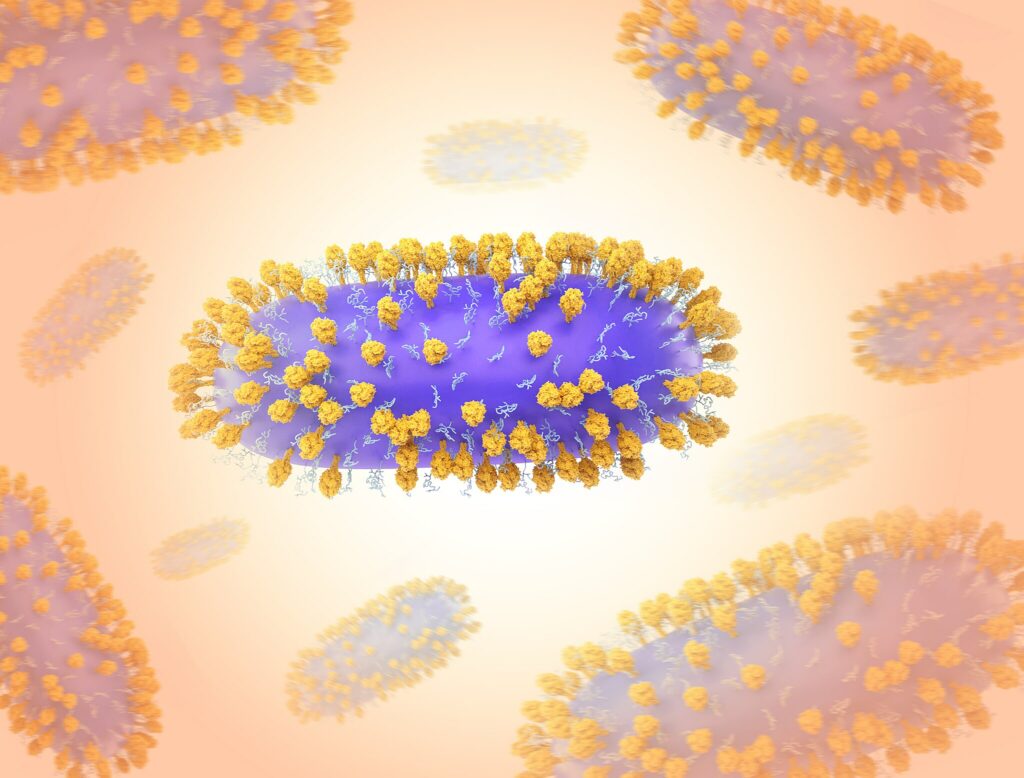
In mid-August, the US Centres for Disease Control and Prevention (CDC) announced: “A new variant of SARS-CoV-2 called BA.2.86 was detected in samples from people in Denmark and Israel. At least two cases have been identified in the United States. This variant is notable because it has multiple genetic differences from previous versions of SARS-CoV-2.”
In fact there are 35 mutations on the spike protein compared to currently circulating variants. That’s as big of a difference as there was between the original virus and the omicron variant identified in November 2021.
The spike protein is what the virus uses to enter our cells. Those mutations could potentially help the virus evade the protection provided by COVID vaccinations and prior infections, says Katelyn Jetelina, an epidemiologist and scientific consultant to the CDC, who writes the “Your Local Epidemiologist” blog.
The CDC and the World Health Organization are taking a closer look.
There’s not yet enough data to assess the potential of this variant to cause a wave. But the CDC said last Wednesday that, “based on what [it] knows now, existing tests used to detect and medications used to treat COVID-19 appear to be effective” for the variant.
The CDC also believes that BA.2.86 may be more capable of causing infection in people who have previously had COVID-19 or who have received COVID-19 vaccines because the mutations on the spike protein could allow it to evade our immune systems despite prior vaccinations and having had COVID-19. Scientists are evaluating the effectiveness of the new booster expected to be approved by mid- September.
And companies that make antigen tests, vaccines and treatments are testing them to see if they are effective on the variant.
If the conclusion is that this variant poses a significant risk of triggering waves of cases due to its mutations, it will get its own name. That name, next in the Greek alphabet for COVID variants, would be pi.
/////
Three-and-a-half years since SARS-CoV-2 spread around the world, scientists are still documenting the virus’ myriad effects on human health. What’s clear already is that those effects can continue long beyond the original infection.
Now, researchers have attempted to quantify this long-term harm using a massive database of U.S. veterans’ health records. They found a dramatically increased risk of dozens of conditions including heart failure and fatigue, sometimes years post infection. Overall, the team estimates, COVID-19’s public health impact is more than 50% greater than that of cancer or heart disease. www.science.org/content/article/covid-19-boosts-risks-health-problems-2-years-later-giant-study-veterans-says?
Other researchers say the conclusions broadly reflect what physicians have seen. However, several cite drawbacks in the study’s statistical analysis that could have led it to overestimate harm to the general population.
To assess COVID-19’s impact, Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis and the VA Saint Louis Health Care System, and colleagues analysed data from the U.S. Department of Veterans Affairs. In previous studies of this data set, the same researchers identified an elevated risk of heart attack and mental health disorders up to a year after infection.
This time, the team looked at 80 health problems—from fatigue and other symptoms commonly associated with Long Covid to neurodegenerative disease—and general risk of death or hospitalization up to 2 years post infection. They included data from about 140,000 people who tested positive for SARS-CoV-2 in 2020 and 6 million people with no record of infection that year.
In the 3 months post infection, people who’d had COVID-19 had higher rates of death and many health conditions including heart failure, diabetes, Alzheimer’s disease, and depression. The differences between groups declined over time. Yet even among people who weren’t hospitalized, the risks for about one-third of the health problems studied remained elevated 2 years later, the researchers report today in Nature Medicine. These people had about a 13% increased risk of diabetes compared with the no-infection group, for example.
The figures were starker for people hospitalized with COVID-19: Two years post infection, this group had elevated risks for about two-thirds of the outcomes studied. Compared with controls, they were about 50% likelier to suffer heart failure and more than twice as likely to receive an Alzheimer’s diagnosis.
“This is a rigorous study that matches what we’ve been hearing from [clinicians and patients] for years,” says Francesca Beaudoin, a clinical epidemiologist at the Brown University School of Public Health who was not involved in the work. Although COVID-19 is directly causing some of these health problems, she adds, it could exacerbate others or accelerate their onset.
Al-Aly’s team also translated its results into disability-adjusted life years (DALYs), a measure of healthy lifetime lost because of disease or disability. (The metric, although controversial because of assumptions it makes about how disability affects quality of life, is used in policymaking to quantify public health impact.) The team calculated that SARS-CoV-2 infection led to over 80 DALYs per 1,000 people who weren’t hospitalized, and more than 640 DALYs per 1,000 people who were. Cancer and heart disease each have DALYs of about 50, says Al-Aly, who consults for Gilead Sciences. “Eighty is an astronomically high number.”
However, some scientists say it’s hard to extrapolate from the study’s patient pool to the general population. People who caught SARS-CoV-2 in 2020 were unvaccinated and would have had earlier variants of the virus, not the ones circulating now. What’s more, the veteran population was about 90% male, 70% white, and had an average age over 60.
“[Older] men are some of the people most afflicted by acute COVID,” says Shawn Murphy, a neurologist and bioinformatician at Harvard Medical School and Massachusetts General Hospital. Although the authors tried to correct for this statistically, still, “We need to be careful about doing these extrapolations.”
There are other potential sources of bias, too. It’s unlikely everyone in the “uninfected” group—98% of people in the study—actually avoided infection all year, van Smeden says. Some probably had mild cases that didn’t require health care. If so, the “infected group” really means “people who had more severe infection,” which could magnify COVID-19’s lingering harms, he says.
The infected group may also have been on average less healthy than controls, says epidemiologist Justin Lessler of the University of North Carolina at Chapel Hill. He notes, for example, that hospitalized patients were five times likelier to be diagnosed with tobacco use disorders in the 3 months following infection. He doubts COVID-19 caused them to start smoking—some probably smoked before or would have started anyway. “What we may be seeing here is … people with poor health who are having severe COVID and continue to have poor health afterward.”
Duke University statistician Fan Li adds that greater use of health care—a typical consequence of getting COVID-19—increases a person’s chances of being diagnosed with other conditions. This also skews apparent differences between infected people and controls, and isn’t adequately addressed in the study, she says.
Al-Aly argues these issues don’t substantially affect the study’s findings, adding the team controlled for as many differences between infected and uninfected people as possible. He says the elevated disease risks are “very likely the result” of SARS-CoV-2 infection and that, if anything, the work underestimated COVID-19’s effects.
Researchers did agree on the seriousness of the virus’ long-term harms, and the importance of studying them. The new paper highlights multiple conditions—including diabetes, neurodegenerative disorders, and muscle diseases—that merit further investigation in connection with SARS-CoV-2 infection, Murphy says.