Article by Lalita Panicker, Consulting Editor, Views and Editor, Insight, Hindustan Times, New Delhi
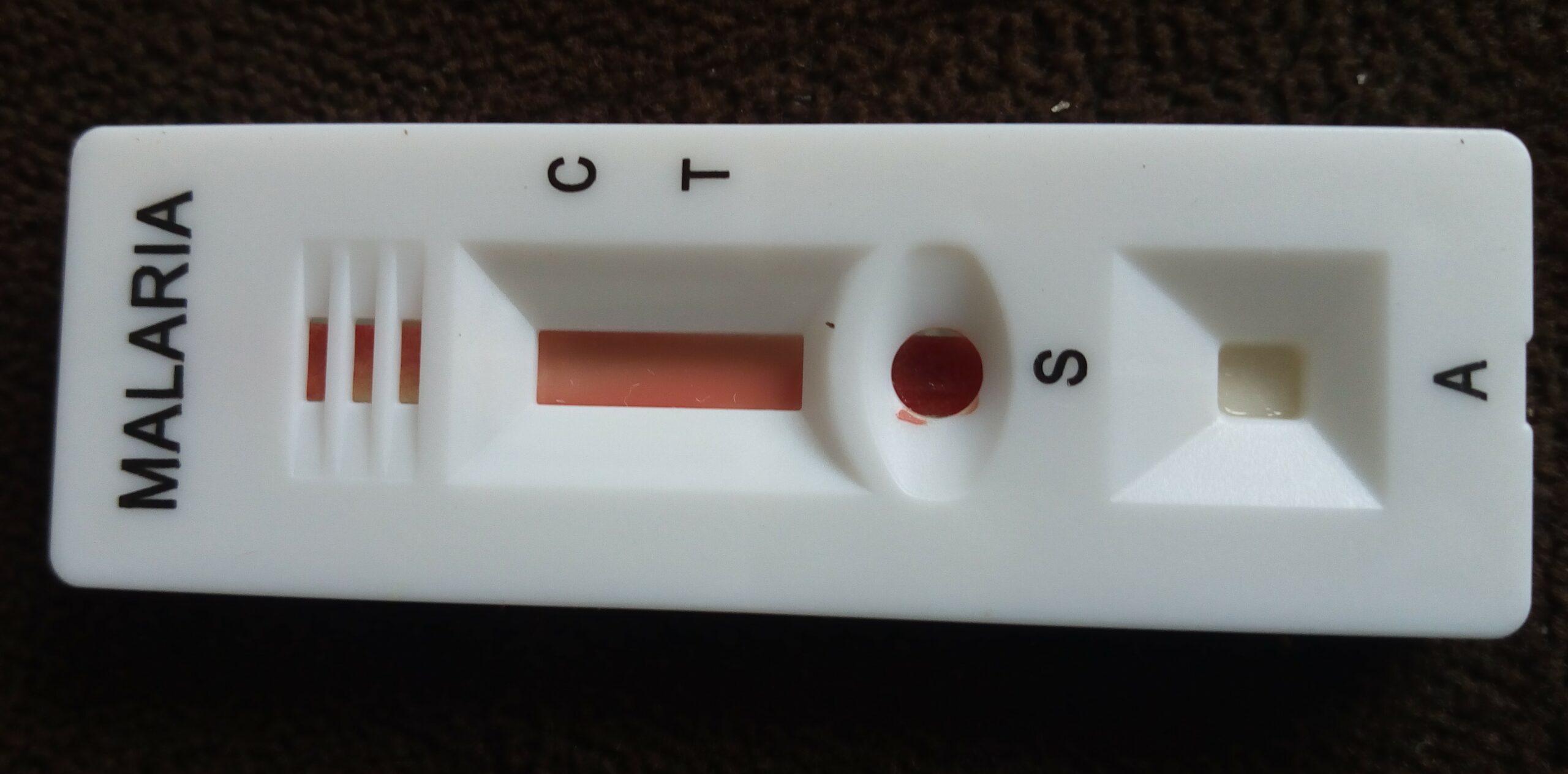
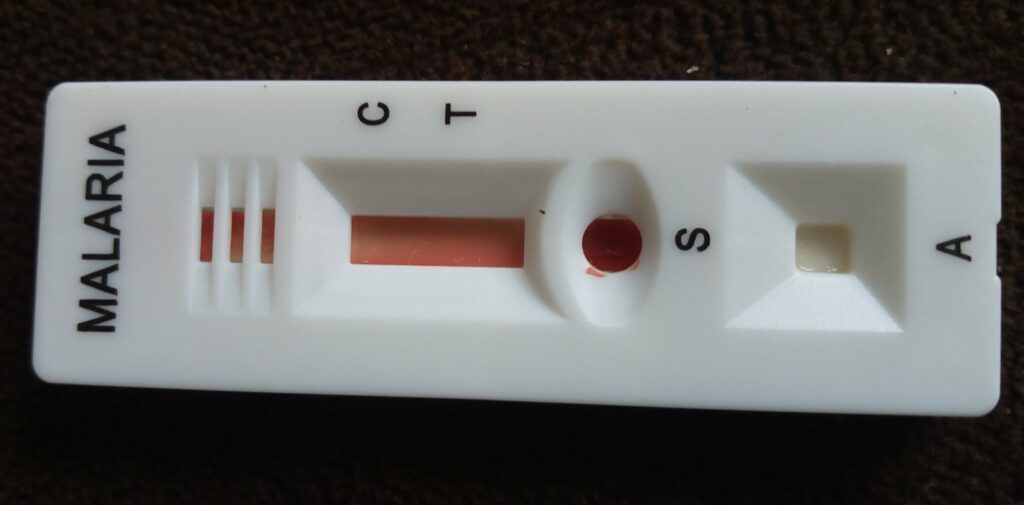
In a major analysis in Africa, the first vaccine approved to fight malaria cut deaths among young children by 13% over nearly 4 years, the World Health Organization (WHO) reported last week. Data from a pilot rollout of the vaccine, called RTS,S or Mosquirix and made by GSK, also showed a 22% reduction in severe malaria in kids young enough to receive a three-shot series. Hundreds of thousands of children are born annually in the parts of Ghana, Kenya, and Malawi included in the analysis, for which WHO revealed the final data at the annual meeting of the American Society of Tropical Medicine and Hygiene. https://www.sciencemagazinedigital.org/sciencemagazine/library/item/27_october_2023/4145583/?Cust_No=60329732
“The RTS,S malaria vaccine is already saving lives,” said John Tanko Bawa, director of malaria vaccine implementation at the non-profit PATH. He added, “What we have seen is a considerable impact of a vaccine described as having modest efficacy.” The 13% drop in deaths is so remarkable that “I was surprised I didn’t hear any gasps when it was stated,” joked medical epidemiologist Mary Hamel, who led the WHO pilot program.
The mortality decline could translate to tens of thousands of lives saved if RTS,S, which WHO approved for widespread use in 2021, is more broadly deployed: In 2021, malaria killed an estimated 468,000 children younger than age 5 in sub-Saharan Africa. Seventeen countries in the region have already won approval to receive doses, which will start to roll out next year.
In trial results published in 2015, RTS,S showed 36.3% efficacy against clinical malaria 4 years after toddlers were vaccinated. In the $70 million pilot, launched in 2019, nearly 2 million children ages 5 months to 24 months have been vaccinated in the three countries, enabling researchers to document the real-world effects of RTS,S and study the impact of its rollout on routine childhood vaccinations.
To calculate mortality, the researchers employed tens of thousands of community reporters who conducted household surveys of deaths in kids younger than age 5. They then compared the death rates between children age-eligible to receive three doses of the vaccine and those who were not, in both RTS,S areas and unvaccinated areas. The comparison, covering 46 months, revealed the 13% decline in mortality—excluding accidental deaths—attributed to RTS,S. The researchers used the same method to detect the 22% decline in severe malaria, counting admissions with severe disease at designated “sentinel” hospitals.
Matthew Laurens, a malaria vaccine researcher at the University of Maryland School of Medicine, calls the results “fantastic news” and theorizes that beyond preventing malaria, the RTS,S vaccine may be broadly “training” the immune system, providing a protective benefit against other infections. Measles and tuberculosis shots have shown such general survival benefits.
Using RTS,S did not hurt uptake of other childhood vaccines or reduce bed net use. But some public health leaders worry its use will require trade-offs. “We are still struggling to implement the tools that we [already] have in many countries,” David Walton, U.S. global coordinator for the President’s Malaria Initiative, told the panel that presented the data last week, noting that the extra cost of RTS,S, at $10 a dose, “is formidable for many countries.” A second malaria vaccine called R21 won WHO authorization earlier this month and is likely to be available more cheaply and in greater quantities than RTS,S.
////
Belgium wants to temporarily ban the use of Novo Nordisk’s diabetes drug Ozempic as a weight loss treatment amid a shortage of the medicine, the Belgian health minister said last Monday. https://www.medscape.com/s/viewarticle/997659?ecd=wnl_edit_tpal_etid5994293&uac=398271FG&impID=5994293
“We have told doctors that they must reserve this drug for their patients who have type 2 diabetes but we see that this strategy does not work,” Belgian federal health minister Franck Vandenbroucke told Belgian broadcaster RTBF.
“I know that this drug can also be useful for people who suffer from morbid obesity so we obviously need to discuss it. But I am convinced that we need a strong and legal signal because simple recommendations are not enough,” he said.
Vandenbroucke said a ban would be temporary and last a few weeks or a few months, as is necessary depending on production and availability of the drug.
Ozempic has overtaken the weight-loss industry. Known generically as semaglutide, the drug was first approved by the U.S. Food and Drug Administration (FDA) in 2017 for adults with type 2 diabetes. But in the last year, its popularity has skyrocketed thanks to its dramatic effects in helping people shed pounds faster than ever. At the same time, Ozempic has faced unprecedented controversy, as this heightened demand has led to dangerous shortages and new stories of serious side effects. Now, some officials are taking a stand against the medication.
https://bestlifeonline.com/ozempic-ban-belgium-news/
The popularity surrounding Ozempic’s weight-loss abilities previously prompted officials in Canada to take action. Back in the spring, British Columbia began restricting the sale of the diabetes drug after U.S. residents started seeking prescriptions in Canada, The Wall Street Journal reported. The province’s health ministry said that it would bar doctors and pharmacists from dispensing Ozempic to people who don’t live in Canada.
“We are ensuring the continued availability of Ozempic,” Adrian Dix, British Columbia’s health minister, told The Wall Street Journal at the time. “We don’t want to become a supplier for the U.S. market.”
Demand for Ozempic has overwhelmed supply in the U.S. The semaglutide injection is currently on the FDA’s Drug Shortages list, with the agency estimating that “limited availability” will last at least through the end of 2023. If you look at the data, that shouldn’t come as a surprise.
A recent report from Trilliant Health revealed that U.S. health care providers wrote more than nine million prescriptions for Ozempic and similar diabetes drugs like Wegovy in the last three months of 2022—reflecting a quarterly increase of 300 percent for these prescriptions.
As in many other countries, the Ozempic shortage in the U.S. is hurting patients who use the drug for their diabetes. Ozempic is not approved for weight loss by the FDA, but providers can prescribe it “off-label” as a weight-loss treatment instead of a diabetes treatment, CNN reported.
In the UK, doctors and prescribers, including private online pharmacies, were ordered to stop prescribing Ozempic to people who don’t have type 2 diabetes as soon as possible. They are also banned from starting new patients with type 2 diabetes on the medicine for as long as the shortage lasts.
////
The COVID-19 treatments millions of Americans have taken for free from the federal government will enter the private market next week with a hefty price tag.
Pharmaceutical giant Pfizer is setting the price for a five-day treatment of Paxlovid at $1,390, but Americans can still access the pills at no cost — for now. The less commonly used COVID-19 treatment Lagevrio, manufactured by Merck, will also hit the market next week. https://apnews.com/article/covid19-paxlovid-treatment-coronavirus-drugs-5ea6124208e915382c40303bd6d749ef
Millions of free, taxpayer-funded courses of the pills will remain at pharmacies, hospitals and doctor’s offices across the country, U.S. Health and Human Services officials said Friday.
The U.S. government initially inked a deal with Pfizer to pay more than $5 billion for 10 million courses of Paxlovid in 2021.
Under a new agreement, reached last month between Pfizer and the federal government, people on Medicaid, Medicare or those who are without medical insurance will not pay any out-of-pocket costs for the treatment through the end of next year. The government will also get 1 million treatment courses to keep in its stockpile.
Suppliers to pharmacies, doctor’s offices and hospitals can begin ordering the treatments from the drug companies starting next week.
////
The only cure for painful sickle cell disease today is a bone marrow transplant. But soon there may be a new cure that attacks the disorder at its genetic source.
Advisers to the Food and Drug Administration will review a gene therapy for the inherited blood disorder, which in the U.S. mostly affects Black people. Issues they will consider include whether more research is needed into possible unintended consequences of the treatment. https://apnews.com/article/sickle-cell-gene-therapy-crispr-8ded5e3a35b30bd257ac756f8a223c51
If approved by the FDA, it would be the first gene therapy on the U.S. market based on CRISPR, the gene editing tool that won its inventors the Nobel Prize in 2020.
The agency is expected to decide on the treatment in early December, before taking up a different sickle cell gene therapy later that month.
Dr Allison King, who cares for children and young adults with sickle cell disease, said she’s enthusiastic about the possibility of new treatments.
The disorder affects haemoglobin, the protein in red blood cells that carries oxygen. A genetic mutation causes the cells to become crescent-shaped, which can block blood flow and cause excruciating pain, organ damage, stroke and other problems.
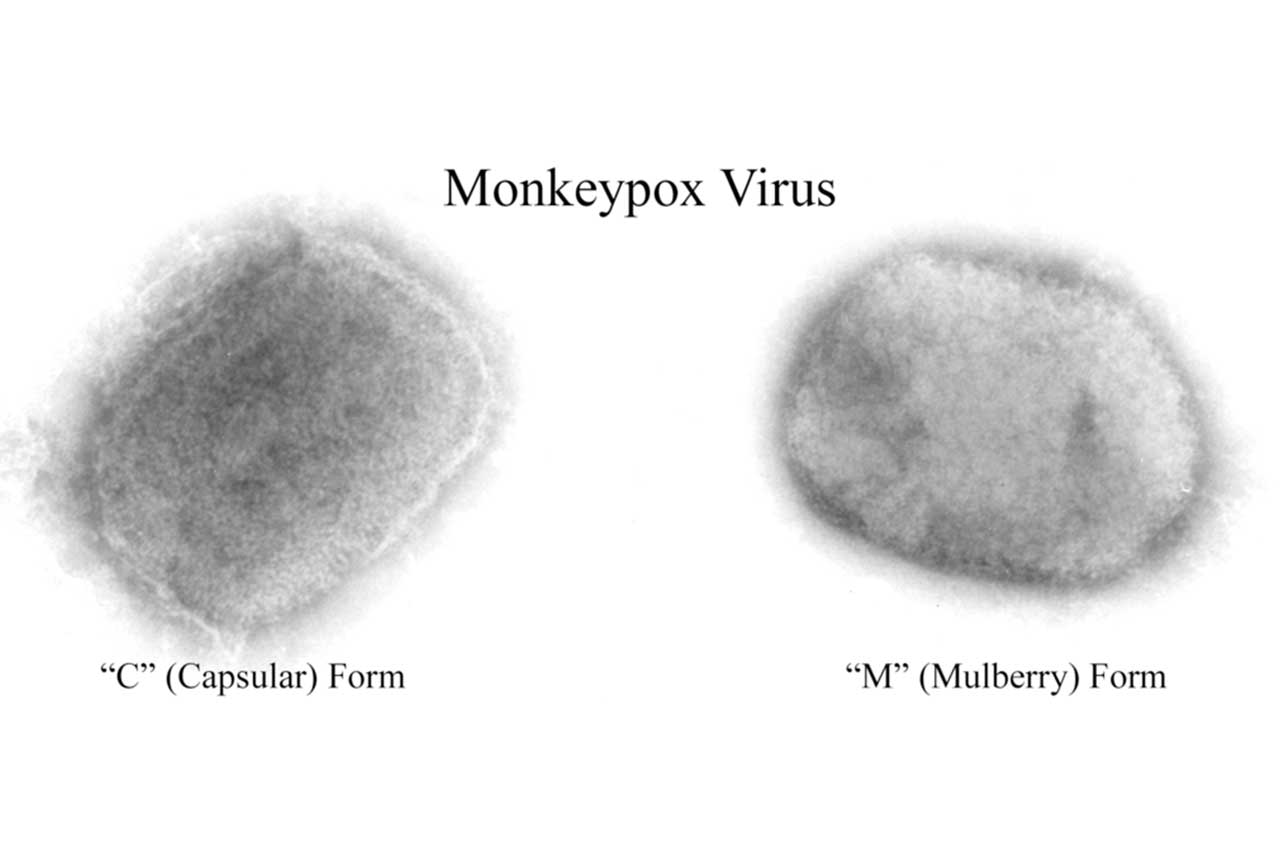
Millions of people around the world, including about 100,000 in the U.S., have the disease. It occurs more often among people from places where malaria is or was common, like Africa and India, and is also more common in certain ethnic groups, such as people of African, Middle Eastern and Indian descent. Scientists believe being a carrier of the sickle cell trait helps protect against severe malaria.
No donor is required for the one-time gene therapy, “exa-cel,” made by Vertex Pharmaceuticals and CRISPR Therapeutics. This new treatment involves permanently changing DNA in a patient’s blood cells.
The goal is to help the body go back to producing a foetal form of haemoglobin — which is naturally present at birth but then switches to an adult form that’s defective in people with sickle cell disease.
When patients undergo the treatment, stem cells are removed from their blood and CRISPR is used to knock out the switching gene. Patients get medicines to kill off other flawed blood-producing cells and then are given back their own altered stem cells.
The treatment has been tested in a relatively small number of patients thus far, the non-profit Institute for Clinical and Economic Review said in an evidence report.
Victoria Gray, of Mississippi, the first patient to test the treatment, shared her experience with researchers at a scientific conference earlier this year. She described suffering with terrible bouts of pain since childhood and receiving high-dose pain medications and sometimes blood transfusions. She described feeling she “was being reborn” the day she got the gene therapy.
But the FDA is asking an outside panel of gene therapy experts next week to discuss a lingering issue that often comes up when discussing CRISPR: the possibility of “off-target effects,” which are unexpected, unwanted changes to a person’s genome. The FDA is looking for advice on whether the company’s research on such effects was adequate to assess the risk or whether additional studies are needed. While the agency doesn’t have to follow the group’s advice, it often does.
The FDA is expected to decide on the second gene therapy for sickle cell, made by Bluebird Bio, before the end of the year. Bluebird’s treatment works differently. It aims to add functional copies of a modified gene, which helps red blood cells produce “anti-sickling” haemoglobin that prevents or reverses misshapen cells.
The companies have not released potential prices for either therapy, but the institute report said prices up to around $2 million would be cost-effective. By comparison, research earlier this year showed medical expenses for current sickle cell treatments, from birth to age 65, add up to about $1.6 million for women and $1.7 million for men.