Africa faces new challenges in its fight against malaria: the climate is becoming more mosquito friendly just as the insects are evolving to evade the insecticides and the malaria parasites are becoming resistant to medicines that have brought down deaths. In 2020, the World Health Organization estimated approximately 90% of malaria cases and 92% of deaths occurred in Africa. Over 600,000 African children died of malaria in that year alone.
This article uses Rwanda, a small and landlocked central African nation, to illustrate the struggle between governments and insects.
Progress in fighting malaria
There has been huge progress in malaria control since 2000. In the last 20 years, more than 600 million malaria cases and more than 6 million deaths have been averted. This progress has been made through unprecedented political commitment and partnerships. However, progress has slowed since 2016. In 2022, the fight against malaria faces new and growing challenges. Better data confirms the global malaria burden is higher than previously estimated and COVID-19 and other challenges such as increasing drug and insecticide resistance and humanitarian emergencies led to an increase in malaria deaths for the first time in over a decade.
Take Rwanda as an example. According to data from the Rwanda Biomedical Centre (RBC), the country saw a decrease in the prevalence of malaria, where cases declined from 5 million to 1 million over a five-year period, from 2016 to 2021. Severe malaria cases also dropped from 18,000 to fewer than 2,000, and the number of deaths related to malaria shrunk from 700 to 69.
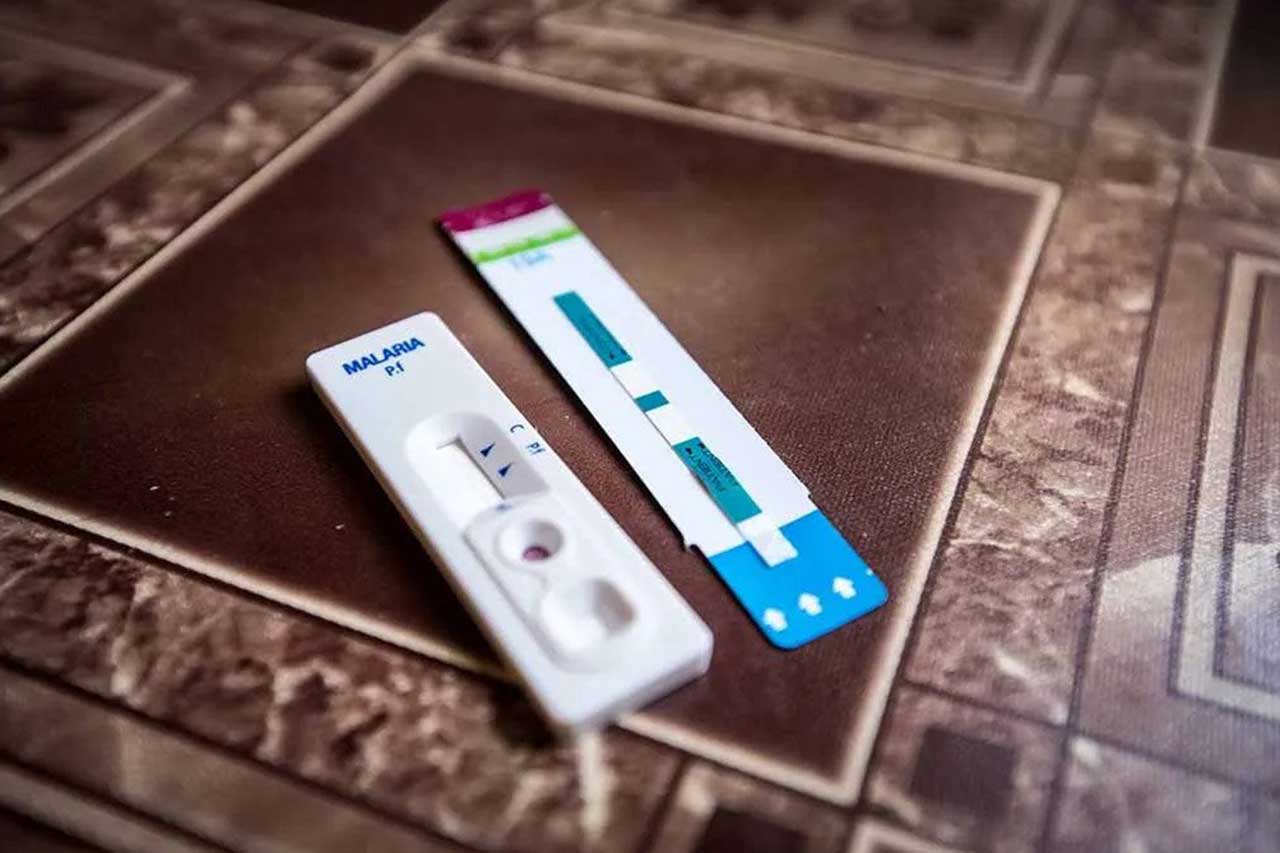
The accomplishments were made possible by a variety of factors, including RBC’s interventions to ensure that services for diagnosing and treating malaria are made more accessible to the public. Currently, up to 60% of all malaria cases are diagnosed and treated at home by community health workers.

In the past, the government rolled out indoor residual spraying campaigns, where trained staff sprayed insecticides inside residential homes to get rid of mosquitoes, as well as the use of drones for spraying outdoor mosquito breeding grounds. Dr Aimable Mbituyumuremyi, the Division Manager for malaria and other parasitic diseases at RBC in 2021, said that drones helped in the precision mapping of mosquito breeding sites and in spraying the larvicide.
Rwanda joined the Zero Malaria Starts with Me movement in 2020 as part of efforts to eradicate the disease. The campaign was launched in 2018 by Rwanda’s President Paul Kagame, in his role then as Chair of the African Union, to build community ownership of malaria efforts and increase political commitment for malaria elimination. So far, 25 countries have launched the movement. Progress was not unique to Rwanda alone, as, throughout Sub-Saharan Africa, there have been symbiotic efforts to tackle malaria head-on by investing in communities and health systems and rolling out innovative and integrated programmes to defeat this millennia-old disease. Such cases show that malaria can be eliminated. However, the fight against malaria remains a tough battle, especially in Sub-Saharan Africa.
Lockdowns and climate change have helped mosquitoes
According to the results of the World Health Organization’s survey, many countries in Sub-Saharan Africa experienced disruptions in malaria prevention, diagnosis and treatment services during the first quarter of 2021. Lockdowns and restrictions on the movement of people and goods led to delays in the delivery of insecticide-treated mosquito nets or indoor insecticide spraying campaigns. Although, malaria programmes did a great job in continuing services as much as possible and avoided the direst of predictions in terms of the impact of COVID.

However, some of the factors responsible for malaria deaths are long-term and include population and demographic dynamics; and; human activities such as deforestation, irrigation and swamp drainage. These add to the existing factors on the continent, such as weak and under-resourced health systems, human resources limitations, remaining critical gaps in access to malaria control services and poor surveillance systems.
The situation could get worse, as recent data from the United Nations shows that there is a complex relationship between malaria and climate change, which could soon put millions more at risk of the disease.
Climate change is often characterized by increasing temperatures, a surge in natural disasters, locust invasions, floods, drought, and so on. With warmer temperatures and variations in rainfall, researchers from the University of Florida expect that malaria vulnerable areas will change and the total transmission zone will expand. At higher altitudes, the malaria-carrying female anopheles mosquito multiplies, which could result in an increase in malaria transmissions in areas where it was not even reported before. As malaria arrives in new areas or in tropical and temperate countries that have, either eliminated or controlled transmission, this presents a significant risk to populations never exposed to the malaria parasite as they lack protective immunity. For example, districts in Rwanda’s Northern Province and Kigali are not generally known for epidemics but are most likely prone based on altitude and climate conditions.
Although researchers are not yet sure of how dramatic the impact of climate change will be on malaria, it’s clear that its influence, as well as other environmental factors on vector-borne disease, is a significant threat that could be prevented with the right strategies and consistent approach.
Therefore, there is an ardent need for adequate and equitable investments in research and monitoring exercises, to identify how climate may impact upon malaria control and elimination programmes and to identify regions where climate conditions may become suitable for resurgence or spread. This could help provide current and improved treatment to those who are most vulnerable and to monitor how the distribution of the disease is changing.
Resistance to insecticides and medicines
Hundreds of thousands of people died from malaria after resistance developed to the treatments in the second half of the 20th century. At that time, there was no meaningful research and development (R&D) pipeline for new antimalarials to replace them until artemisinin-containing combinations were introduced at the turn of the century. Innovations in treatment, along with the widespread use of tools such as long-lasting insecticide-treated nets and rapid diagnostic tests, have helped save more than seven million lives and prevent more than one billion new malaria infections since the early 2000s. Currently, the WHO recommended first-line treatment, artemisinin-based combination therapies (ACTs), are largely effective and well tolerated and have been used for almost 20 years. However, the emerging threat of resistance demands urgent action to develop new medicines with novel and distinct mechanisms of action.
Emerging resistance to artemisinin has been observed in the Greater Mekong region and spontaneous resistance is now increasingly seen in Africa in Eritrea, Ethiopia, Rwanda, Somalia, Sudan, Uganda, and with increasing frequency in the Horn of Africa. Currently artemisinin resistance means that each patient must take more tablets, but if parasites also become resistant to the partner drug, then the treatment will become ineffective, leading to many deaths.
As well as resistance to treatment, a different kind of resistance is emerging rapidly to a vital line of defence in malaria: insecticides. Failure to monitor, mitigate and manage insecticide resistance will likely result in an increase of malaria cases and deaths. This is particularly worrisome in the case of pyrethroids, the insecticide used on insecticide-treated bed nets (ITNs). The growing inability of insecticides to kill malaria vectors is concerning because insecticide-based interventions are vital to preventing death and disease from malaria in African children. ITNs are estimated to be responsible for 78% of the 663 million clinical malaria cases averted in sub-Saharan Africa since 2001, and more than 50% of people in malaria-endemic areas in sub-Saharan Africa slept under ITNs in 20161.
Vaccines
In 2021, the WHO recommended withe despread use of the world’s first malaria vaccine for children. Although this is a major breakthrough in child health, the vaccine is yet to reach the most affected regions in Sub-Saharan Africa. Despite the recent announcement by UNICEF to supply 18 million doses of RTS,S/AS01 (RTS,S) through a contract with GSK, even with this announcement, supply will continue to be limited at first and will only increase over time as manufacturing capacity ramps up to the level required.

Rwanda is in a unique position to become a leader, as the country is home to the first of three planned mRNA vaccine manufacturing facilities across Sub-Saharan Africa. This development has the potential to make Rwanda a leader in vaccine R&D and manufacturing for the continent, especially as these new technologies are applied to the malaria fight.
“What got us here …will not get us where we need to be”
At the recent Commonwealth Head of Government meeting in Kigali, the leaders called out the opportunity to accelerate the fight against infectious diseases, including malaria. Kenya’s President, who also doubles as the Chair of the African Leaders Malaria Alliance, President Uhuru Kenyatta, in his opinion piece after the meeting, highlighted the need for vaccines and investment to tip the scales against malaria. “…. what got us here in the fight against malaria will not get us where we need to be in 2030. We need fresh tools, such as the new malaria vaccine, RTS, S. We must ensure that everyone, everywhere, can have access to tools, which prevent the disease, such as mosquito nets, indoor residual spraying and seasonal chemoprevention. We must also ensure that when people get sick, they can get treatment as soon as they need it.”
By Immy Mulekatete
Communications, Media and Marketing Enthusiast