Article by Lalita Panicker, Consulting Editor, Views, Hindustan Times, and Editor, Insight, Hindustan Times, New Delhi
Last month, the World Health Organization (WHO) revealed that the Democratic Republic of the Congo (DRC) was experiencing its largest, most deadly outbreak of mpox ever, with more than 12,000 suspected cases so far this year and nearly 600 deaths, far surpassing those from the global outbreak of the same viral disease over the past 2 years. The WHO report and a study out on 29 November also explore a worrisome possibility: that the strain of virus in the DRC, far deadlier than the one that drove the global outbreak, is in some cases spreading between sexual partners. https://www.science.org/content/article/congos-deadliest-mpox-outbreak-new-worry-virus-has-become-sexually-transmissible?
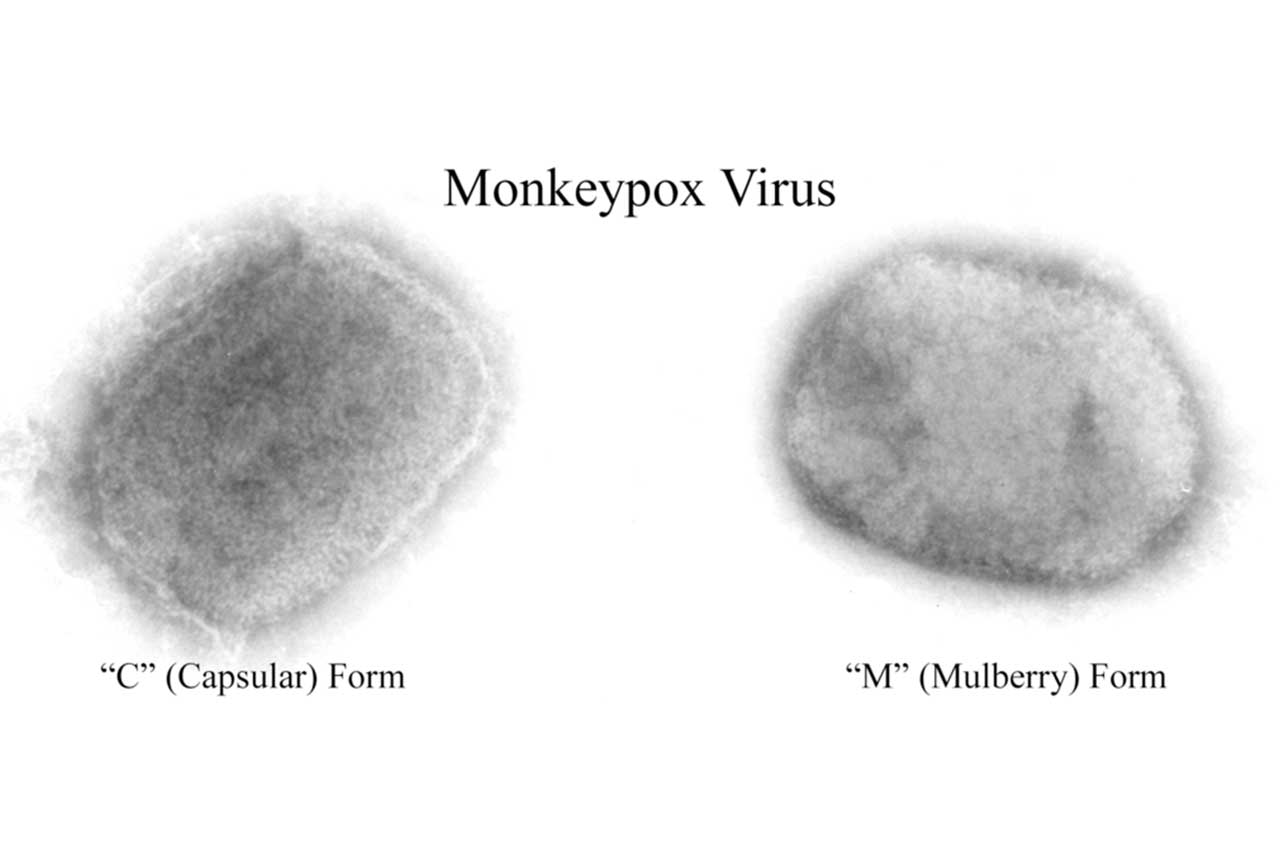
Originally known as monkeypox, the disease is caused by a virus (MPXV) that long has sporadically infected people in rural areas of the DRC, mostly though contact with infected squirrels and other rodents. Researchers have documented occasional spread among household contacts, but the MPXV strain in the DRC, designated clade I, has never been linked to sexual transmission, a major mode of transmission for the clade IIb strain in the global outbreak. Researchers are now rushing to analyse the latest DRC cases to see whether the local virus has changed genetically, and some scientists suggest the country should consider at least targeted use of the mpox vaccines that are now widely available in wealthy countries outside of Africa.
It’s “shocking” that the vaccination is not yet accessible in DRC,” says Yale University epidemiologist Gregg Gonsalves. “As a question of equity, it’s hard to stomach.” Gonsalves went to the DRC in the spring to help model how much vaccine the country would need to combat mpox, but the recent revelation that MPXV might be spreading sexually there “scrambles things a bit,” he says.
MPXV typically produces skin blisters and lesions and can cause particularly severe disease in immunocompromised people. The first human case of mpox was detected in 1970 in the DRC, and until recently it was only endemic in sub-Saharan African countries. (WHO renamed the disease because of concerns that monkeypox was “racist and stigmatizing” language.) But last year, more than 85,000 cases occurred outside of Africa, primarily among men who have sex with men (MSM), leading WHO to ring its loudest alarm, a Public Health Emergency of International Concern.
Now, the same pattern of transmission may have emerged with the more deadly virus. WHO’s 23 November Disease Outbreak News and a study posted today(29 November) in Emerging Infectious Diseases (EID) conclude that clade I MPXV is being passed on sexually among MSM and sex workers in the DRC. The studies describe two clusters, one among MSM and one among 20 sex workers. “Is this something new or something that we’ve been missing?” asks University of Manitoba virologist Jason Kindrachuk, who co-leads the International Mpox Research Consortium and is the corresponding author of the EID paper.
Eddy Kinganda-Lusamaki, a clinician based at the DRC’s National Institute of Biomedical Research (INRB) who co-authored the EID report, says improved surveillance could account for some of the unprecedented surge in the DRC cases and deaths, which WHO puts at 581 this year. “Monkeypox surveillance was at some point neglected in our country because of lack of resources to investigate,” says Kinganda-Lusamaki, who is working on a Ph.D. in virology at the University of Montpellier. But he doesn’t think surveillance is the whole story. “Cases have been detected in areas that did not report cases in the past,” he notes, including Kinshasa, a city of 17 million people that has far more accessible health care than the rural communities traditionally hit hardest by mpox.
Epidemiologist Anne Rimoin of the University of California, Los Angeles, another EID co-author, has studied mpox in the DRC for 2 decades and says it’s unclear whether sexual transmission made a significant contribution to the apparent explosion in cases—or whether it’s truly even a new phenomenon in the country. “If you’re not looking for it, you’re unlikely to find it,” Rimoin says. She adds that people with genital lesions may not seek care, especially if they are MSM or sex workers. “There’s stigma associated with transmission in this manner, so it’s going to be very hard to document,” she says.
Rimoin also notes that the vast majority of cases have not been confirmed by polymerase chain reaction (PCR) tests that detect genetic signatures of the viruses. “That’s going to be really important to parse out,” she says. Virologist Martine Peeters, Kinganda-Lusamaki’s Ph.D. adviser, says her lab has a new test that can confirm infections that PCR misses by looking for antibodies to MPXV, which last longer in the blood than the virus. “Maybe there are more asymptomatic or post symptomatic cases, which means [the DRC tally] may even be underreported,” she says.
The EID and WHO reports offer different and somewhat conflicting details about the MSM cluster. WHO says the first sexually transmitted case traces back to a resident of Belgium who arrived in Kinshasa on 15 March with “anal itching and discomfort,” but the next day travelled to a town 260 kilometres away. He sought medical care there a week later, and tests sent to INRB confirmed he had mpox and that it was clade I virus. An epidemiological investigation found that the man had sex with four men and one woman who later tested positive themselves.
The EID report describes the same cluster differently, saying the first mpox diagnosis was a Congolese man who reported having sex in Europe with a man who frequently visited the DRC and had mpox symptoms. The report describes the virus from the original DRC man and four of his contacts who became infected. “We need to better investigate and better characterize what’s going on and what has circulated,” says Kinganda-Lusamaki, who is not convinced the cluster started with a man infected in Europe. “It’s more likely that the patient got infected in the country [DRC],” he says. “We are still at the level of hypothesis.”
For the clade IIb virus that spread globally, genetic analyses showed that several mutations likely explained how it had changed to transmit more readily through sex. But there’s no evidence yet that the viruses isolated from the DRC cases have undergone the same changes. “The analysis is not that easy,” Peeters says.
When clade IIb surfaced in MSM in Europe and North America last year, there was an immediate demand for a smallpox vaccine made by Bavarian Nordic that the U.S. Food and Drug Administration had approved for mpox. The company’s CEO, Paul Chaplin, says the DRC has never requested the vaccine. “Bavarian Nordic has not been approached by any African country” for doses, Chaplin says. WHO has a multistep process that gives a stamp of approval to vaccines for use worldwide, and Chaplin says the company has filed the initial paperwork with the agency but has yet to hear back. The company, he says, “is willing to support the current situation in the DRC.”
////
Eli Lilly (LLY.N) said on Friday (01 Dec) the U.S. Food and Drug Administration (FDA) gave a second approval for its drug Jaypirca, which is used to treat a form of blood cancer. https://www.reuters.com/business/healthcare-pharmaceuticals/us-fda-gives-second-approval-eli-lillys-drug-type-blood-cancer-2023-12-01/
The company said the health regulator gave the new approval to the drug for the treatment of chronic lymphocytic leukaemia (CLL), a type of cancer in which the bone marrow makes too many of certain white blood cells.
Jaypirca was first given accelerated approval by the FDA on Jan. 27 for the treatment of mantle cell lymphoma (MCL), a rare type of blood cancer that starts in white blood cells and spreads to other parts of the body.
MCL is a more aggressive form of cancer compared to CLL, according to the National Institutes of Health.
The drug aims to treat adults with CLL after at least two lines of therapy.
////
Britain said on Monday (27 Nov) it had detected its first human case of flu strain A(H1N2)v, which is similar to a virus currently circulating in pigs, and that the individual concerned had experienced a mild illness and fully recovered. https://www.medscape.com/s/viewarticle/998789?ecd=mkm_ret_231202_mscpmrk-OUS_IntStories_etid6105735&uac=398271FG&impID=6105735
The UK Health Security Agency (UKHSA) said that the case was detected as part of routine national flu surveillance and the source of infection was not known.
“This is the first time we have detected this virus in humans in the UK, though it is very similar to viruses that have been detected in pigs,” UKHSA incident director Meera Chand said.
Close contacts of the case are being followed up by the authorities, the statement said, adding that the situation was being monitored with increased surveillance in surgeries and hospitals in northern England.
In 2009, the swine flu pandemic in humans infected millions of people. It was caused by a virus which contained genetic material from viruses that were circulating in pigs, birds and humans.
The UKHSA said that based on early information the infection detected recently in Britain was different from the 50 or so other human cases of the strain found elsewhere globally since 2005.
////
A machine-learning algorithm called PANDA is rivalling human radiologists when it comes to identifying pancreatic cancer from CT scans. The system, based on artificial intelligence (AI), identified pancreatic lesions with a sensitivity of 92.9% and a specificity of 99.9% across more than 20,500 patients. PANDA surpassed the performance of radiologists by 34% in sensitivity and 6.3% in specificity. Pancreatic cancer often has a poor prognosis because it causes non-specific symptoms and is therefore diagnosed late.
Nature Medicine News & Views | 6 min read
////
Some children with brain tumours might benefit from the precision drug tovorafenib. This oral drug eliminated or shrank brain tumours in two-thirds of the 77 children and young adults enrolled in the FIREFLY-1 trial. The participants all had relapsed or treatment-resistant low-grade gliomas with a mutation in the BRAF gene.
Reference: Nature Medicine paper (17 November)This study was presented at the 2023 Society for Neuro-Oncology Annual Meeting in Vancouver.
////
Researchers have discovered that trans-vaccenic acid (TVA) — a nutrient found in meat and dairy products derived from sheep and cows — promotes the activity of cancer-destroying immune cells. The researchers screened 255 blood nutrients for their role in antitumour immunity and found that TVA activated cytotoxic T cells. When mice with melanoma or colorectal cancer were given a TVA-rich diet, tumour growth slowed compared with a control group. People with lymphoma who have higher levels of TVA in their blood tend to respond better to a type of immunotherapy known as chimeric antigen receptor (CAR) T-cell therapy.
New Scientist | 3 min read (paywall)Reference: Nature paper (22 November)